Managing Illness in School – From A to Z.
Introduction:
Illness is something impacts the majority of children, but usually only for a short period of time. Unfortunately, for some children, it can lead to several periods of absence from school, or, in a worst-case scenario, can lead to a prolonged absence from
school.
When we talk about illness, we are referring to both physical and mental health issues, both of which can display similar patterns of absence.
Illness absence accounts for more absence than any other reasons for absence, both in Bradford, and nationally. In England, illness absence equates to 52% of all absences, whilst in Bradford, it equates to 41% of all absences. Primary Schools and Secondary
schools are impacted slightly differently, with illness absence in secondary schools equating to 47% of absence in England (31% in Bradford), and in Primary schools this equates to 59% of all absence in England (56% in Bradford).
The standard approach to illness absence in schools:
The expectation placed on parents (and hopefully visible in the school’s attendance policy) is that the school should be contacted on the first day of a child’s absence from school, without exception. At this point, a parent should explain to the school
why their child is absent from school, and when they expect the child to return to school. As the data shows, on most occasions, the parent will explain that their child is ill, and so they should be able to provide details on the illness (i.e. the condition
and/or symptoms), and how long they will be absent. It may also be the case that the parent is awaiting contact with their GP surgery to diagnose the illness before being able to provide more details to the school re: the condition and length of time away
from school.
The Department for Education states:
“Schools are not expected to routinely request that parents provide medical evidence to support illness absences. Schools should only request reasonable medical evidence in cases where they need clarification to accurately record absence in the
attendance register – i.e. making a decision that code I is the absence code that accurately describes the reason the pupil is not in school for the session in question. In the majority of cases a parent’s notification that their child is too ill to attend
school will be that evidence and can be accepted without question or concern.”
On this basis, the expectation is that schools will usually record the absence as “Code I – Illness”, which is classed as an authorised absence.
Frequently Asked Question 1 – How do we know how long a child should be absent from school.
The UK Health Security Agency have produced a wealth of information, advice and guidance on this area, both in terms of ensuring child miss as little time from school as possible, but also to help minimise the risk of breakout of infectious diseases.
This poster provides guidance to schools and parents on the length of absence required for most common childhood ailments, and you can click on it to download your own copy.
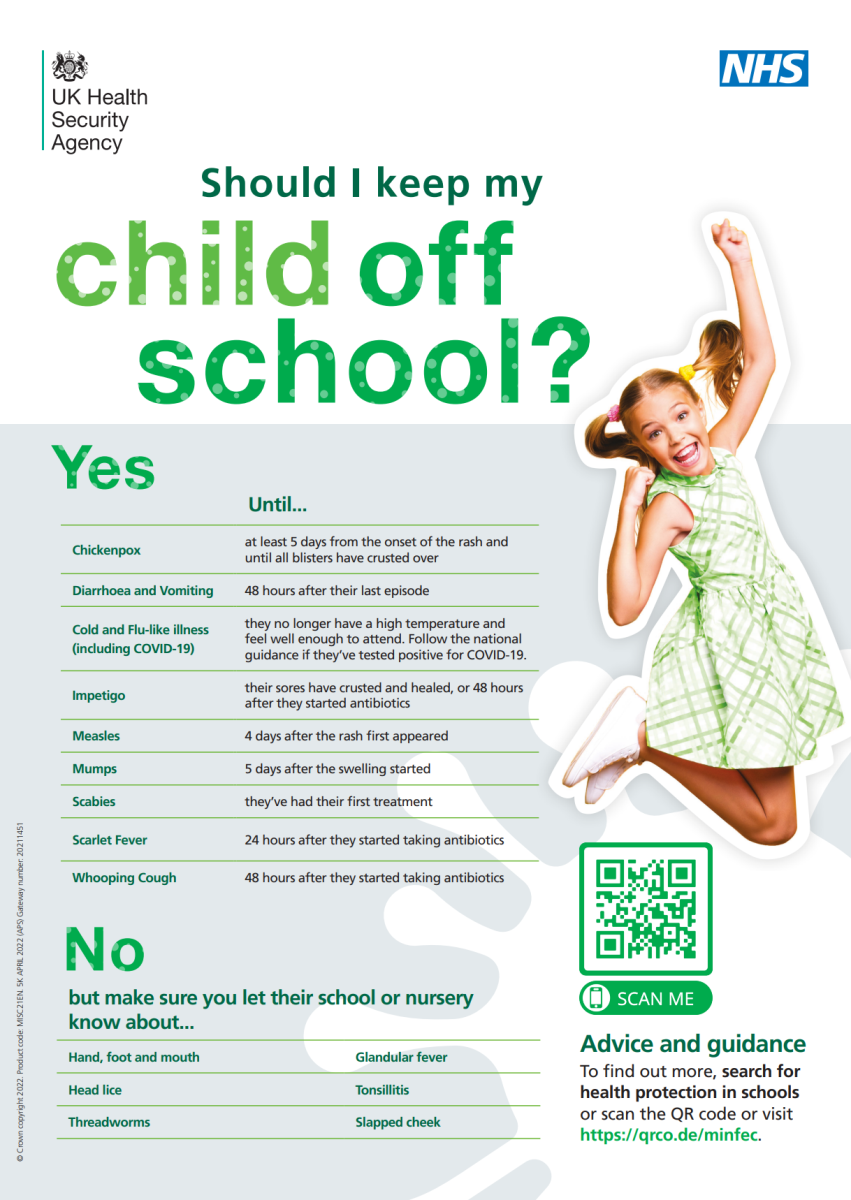
More detail is also available here:
https://www.gov.uk/government/publications/health-protection-in-schools-and-other-childcare-facilities/managing-specific-infectious-diseases-a-to-z , including information on when to contact
Yorkshire and Humber Health Protection Team
Things are a bit more complicated for children with mental health issues. The department for education states:
“Schools should set and maintain high expectations for the attendance, engagement and punctuality of pupils who are anxious about attending school. It is important to recognise that, in many instances, attendance at school may serve to help with
the underlying issue as much as being away from school might exacerbate it, and a prolonged period of absence may heighten their anxiety about attending in future.
School staff will recognise that there can be attendance challenges where a child has a social, emotional or mental health issue, particularly a severe issue for which the child is receiving clinical treatment…
Many children will experience normal but difficult emotions that make them nervous about attending school, such as worries about friendships, schoolwork, exams or variable moods. It is important to note that these pupils are still expected to
attend school regularly.
School staff should work quickly to communicate this expectation to parents/carers, and work together with them to ensure that such circumstances do not act as a barrier to regular attendance. Any associated anxiety about attending should be
mitigated as much as possible by creating a plan to implement reasonable adjustments to alleviate specific barriers to attendance…”
So, in summary, all school staff should be aware of the signs and symptoms of anxiety and mental health issues within children and ensure that discussions take place with the child (if appropriate) and parent so that issues can be discussed as early as possible,
hopefully avoiding the issues escalating into prolonged non-attendance.
More guidance on this can be found within the Responding to emotionally-based school avoidance (EBSA) guidance from Bradford Educational Psychology Team, which can be found here:
https://bso.bradford.gov.uk/content/educational-psychology/responding-to-ebsa---guidance-for-schools
The approach to prolonged/multiple absences from school
The DfE’s statutory guidance for schools and academies on supporting pupils at school with medical conditions provides support to schools on this issue. In summary…
Section 100 of the Children and Families Act 2014 places a duty on governing bodies of maintained schools, proprietors of academies and management committees of PRUs to make arrangements for supporting pupils at their school with medical conditions.
Where illness absence escalates, being able to manage situations to ensure that a child’s access to education remains as unaffected as possible is crucial. A school should already have in place a policy for supporting pupils with medical conditions that
is reviewed regularly and is readily accessible to parents and school staff.
The policy should also cover the process for what happens when a member of staff is notified that a child has a medical condition, and who is then responsible for completing an Individual Healthcare Plan (IHP). Individual healthcare plans can help to ensure
that schools effectively support pupils with medical conditions. They provide clarity about what needs to be done, when and by whom. They will often be essential, such as in cases where conditions fluctuate or where there is a high risk that emergency intervention
will be needed, and are likely to be helpful in the majority of other cases, especially where medical conditions are long-term and complex.
An IHP will include information such as:
-
the medical condition, its triggers, signs, symptoms and treatments;
-
the pupil’s resulting needs, including medication (dose, side effects and storage) and other treatments, time, facilities, equipment, testing, access to food and drink where this is used to manage their condition, dietary requirements and environmental issues,
e.g. crowded corridors, travel time between lessons;
-
specific support for the pupil’s educational, social and emotional needs – for example, how absences will be managed, requirements for extra time to complete exams, use of rest periods or additional support in catching up with lessons, counselling sessions;
| The Health Conditions in Schools Alliance have produced a sample policy which can be downloaded for free via their website:
http://www.medicalconditionsatschool.org.uk . The website also contains an example Individual Healthcare Plan (IHP), together with example IHPs covering a variety of common child health issues i.e. Asthma, Epilepsy etc. |
The process for managing children with medical needs should look something like this:
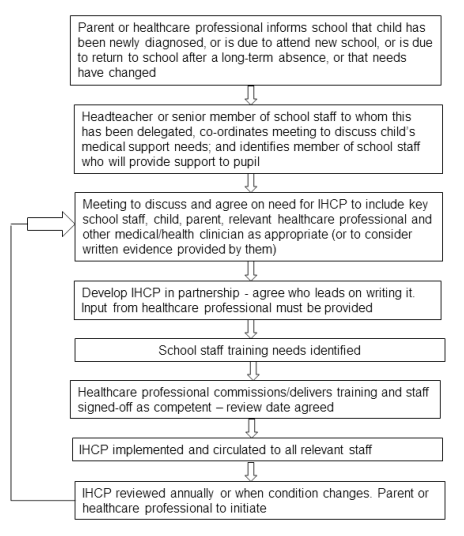
With a Medical Needs Policy and a process and plan for managing Individual Health Care Needs in place, a schools ability to apply it will depend greatly on information about the child’s specific medical needs. Parents and the School Nursing Team have a
key role to play:
“Parents should provide the school with sufficient and up-to-date information about their child’s medical needs. They may in some cases be the first to notify the school that their child has a medical condition. Parents are key partners and should
be involved in the development and review of their child’s individual healthcare plan, and may be involved in its drafting. They should carry out any action they have agreed to as part of its implementation, e.g. provide medicines and equipment and ensure
they or another nominated adult are contactable at all time.”
“Every school has access to school nursing services. They are responsible for notifying the school when a child has been identified as having a medical condition which will require support in school. Wherever possible, they should do this before
the child starts at the school. They would not usually have an extensive role in ensuring that schools are taking appropriate steps to support children with medical conditions, but may support staff on implementing a child’s individual healthcare plan and
provide advice and liaison, for example on training. School nurses can liaise with lead clinicians locally on appropriate support for the child and associated staff training needs; for example, there are good models of local specialist nursing teams offering
training to local school staff, hosted by a local school. Community nursing teams will also be a valuable potential resource for a school seeking advice and support in relation to children with a medical condition.”
“Other healthcare professionals, including GPs and paediatricians, should notify the school nurse when a child has been identified as having a medical condition that will require support at school. They may provide advice on developing individual
healthcare plans. Specialist local health teams may be able to provide support in schools for children with particular conditions (e.g. asthma, diabetes, epilepsy).”
More information about Bradford’s School Nursing Team can be found here:
https://bso.bradford.gov.uk/content/health-including-health-and-safety/the-school-nurse-team-
The information above applies to children with mental health issues in exactly the same way. These children should receive an Individual Healthcare Plan as part of their ongoing support to enable them to continue to access education based on their individual
needs.
Frequently Asked Question 2 – How about children with prolonged/multiple absences from school where we have not been notified about a specific medical condition
The Department for Education states:
“Only where the school has genuine and reasonable doubt about the authenticity of the illness should medical evidence be requested to support the absence.
Where medical evidence is deemed necessary, schools should not be rigid about the form of evidence requested and should speak to the family about what evidence is available. Schools should be mindful that requesting additional medical evidence
unnecessarily places pressure on health professionals, their staff and their appointment system, particularly if the illness is one that does not require treatment by a health professional.
Where a parent cannot provide evidence in the form requested but can provide other evidence, schools should take this into account. Where a parent cannot provide any written evidence, the school should have a conversation with the parent and
pupil, if appropriate, which may in itself serve as the necessary evidence to record the absence.”
Ultimately, if a school feels that it is not in receipt of the necessary evidence to authorise the absence, they should make the parent aware of this, and begin to unauthorise the absence. The parent should be notified in writing as a minimum about this
decision, and we do provide a template letter as part of our Stage One letters within our Staged Intervention Approach to School Attendance -
https://bso.bradford.gov.uk/content/education-safeguarding/attendance/poor-attendance-interventions
Continued unauthorised absence should then be managed in accordance with the staged intervention approach, with schools able to request a legal intervention from the Local Authority where appropriate.
Schools should also be aware of Perplexing Presentations (PP) and Fabricated or Induced Illness (FII) in Children, the details of which can be found within the West Yorkshire Consortium Inter Agency Safeguarding and Child Protection Procedures.
“FII should be considered if a child is being presented as ill when they are not, or as more ill than is actually the case, because of the parent or carer's report or action (usually the mother). Often there is discrepancy between parental accounts
of illness and observations of professionals, and puzzlement within the health team.”
Professionals not from a Health setting including Education/Early years/Early Help/Children's Social Care have the following roles and responsibilities:
-
Professionals may have concerns because parents are describing a child's illness or health needs which are not witnessed by the professionals;
-
In such situations, professionals should consider the other alerting signs in Table 2 - Alerting signs to possible FII. If they remain concerned or have heightened concerns they should discuss the child with their safeguarding lead;
-
If concerns remain, then the child should be discussed with relevant health professionals. This could involve liaison between the service manager and the area Safeguarding Team or the Designated Doctor for Safeguarding Children;
-
Consent from the parents to do this should be sought on the grounds that that this is usual practice where a child has an illness which is impacting on their health or development;
-
At this stage the concern about possible FII should not be disclosed to the parent/carer. If parents refuse consent for a discussion with health professionals then this should be discussed with the safeguarding lead to consider whether refusal increases
the level of concern.
-
When a parent/carer reports restrictions or limitations for normal school activities due to reported 'health' issues, it is important this is verified.
More details can be found here:
https://westyorkscb.proceduresonline.com/p_fab_ind_ill.html
Frequently Asked Question 3 – What about these Sickness Returns? Do we need to notify the LA on every occasion?
The Department for Education states:
“[Schools must provide] the local authority with the full name and address of all pupils of compulsory school age who have been recorded with code I (illness) and who the school has reasonable grounds to believe will miss 15 days consecutively
or cumulatively because of sickness”
All state-funded schools in Bradford provide attendance and absence data automatically through a data feed between the school’s MIS system (ie. SIMS, Arbor, Bromcom etc) and the LA twice daily. This means that the LA is aware of any child who has missed
15 days consecutively or cumulatively because of sickness. The LA then uses this data to inform interventions by either the school’s Attendance Support Team Officer, or by the Medical Needs and Hospital Education Service (MNHES).
Due to this, there is not a need for schools to submit a manual sickness return as the LA is notified automatically on every occasion.
The approach to children with health needs who cannot attend school:
The Department for Education states:
“Where possible, the child’s health needs should be managed by the home school so that they can continue to be educated there with support, and without the need for the intervention of the local authority. However, as soon as it is clear that
the home school can no longer support the child’s health needs and provide suitable education, the school should speak to the local authority about putting alternative provision in place.
There is no absolute legal deadline by which local authorities must start to arrange education for children with additional health needs. However, as soon as it is clear that a child will be away from school for 15 days or more because of their
health needs, the local authority should arrange suitable alternative provision. The 15 days may be consecutive or over the course of a school year.”
As mentioned already, the LA is notified automatically that a child has been absent for 15 days in an academic year due to illness, and the LA, either via MNHES, or via your Attendance Support Team Officer, will speak to you about the child, their individual
healthcare plan, and any support the LA can provide. However, you may wish to speak to MNHES directly to discuss a situation, and their webpage provides details on how to do this:
https://bso.bradford.gov.uk/content/special-educational-needs-and-disabilities/specialist-provision/medical-needs-and-hospital-education-service
Where MNHES puts in place alternative provision for the child, the “main” school remains responsible for maintaining the school register, and should use Attendance Code “K” to record the child’s attendance with MNHES. The school should then apply the relevant
attendance and absence codes for other sessions where the child is not expected to attend MNHES, for example:
-
C2 to record that the child is on a modified timetable agreed between the school, parent, medical professionals (if relevant) and MNHES, and is not expected to attend.
-
Code I to record that the child was due to attend school / MNHES, but was unable to because they were too ill.
At no point is the child dual registered at MNHES, so code “D” cannot be applied.
The following information has been taken from the following statutory and non-statutory guidance:
Department for Education
-
Working Together to Improve School Attendance
https://www.gov.uk/government/publications/working-together-to-improve-school-attendance
-
Letter to school leaders on mild illness and school attendance from the Chief Medical Officer and leading health professionals.
https://www.gov.uk/government/publications/letter-to-school-leaders-on-mild-illness-and-school-attendance
-
Supporting pupils with medical conditions at school
https://www.gov.uk/government/publications/supporting-pupils-at-school-with-medical-conditions--3
-
Education for children with health needs who cannot attend school
https://www.gov.uk/government/publications/education-for-children-with-health-needs-who-cannot-attend-school
-
Promoting and supporting mental health and wellbeing in schools and colleges
https://www.gov.uk/guidance/mental-health-and-wellbeing-support-in-schools-and-colleges
-
Mental health issues affecting a pupil's attendance: guidance for schools
https://www.gov.uk/government/publications/mental-health-issues-affecting-a-pupils-attendance-guidance-for-schools
UK Health Security Agency
-
Health protection in children and young people settings, including education https://www.gov.uk/government/publications/health-protection-in-schools-and-other-childcare-facilities
-
Children and young people settings: tools and resources
https://www.gov.uk/government/publications/health-protection-in-schools-and-other-childcare-facilities/children-and-young-people-settings-tools-and-resources
-
Managing specific infectious diseases – A to Z
https://www.gov.uk/government/publications/health-protection-in-schools-and-other-childcare-facilities/managing-specific-infectious-diseases-a-to-z
City of Bradford Metropolitan District Council
-
Responding to emotionally-based school avoidance (EBSA)
https://bso.bradford.gov.uk/content/educational-psychology/responding-to-ebsa---guidance-for-schools
-
Staged Intervention Approach to School Attendance -
https://bso.bradford.gov.uk/content/education-safeguarding/attendance/poor-attendance-interventions
-
Medical Needs and Hospital Education Service (MNHES)
https://bso.bradford.gov.uk/content/special-educational-needs-and-disabilities/specialist-provision/medical-needs-and-hospital-education-service
Local Government and Social Care Ombudsman
-
Out of school, out of sight? Ensuring children out of school get a good education
https://www.lgo.org.uk/assets/attach/6271/FR-Out-of-School-F.3.pdf
West Yorkshire Consortium Inter Agency Safeguarding and Child Protection Procedures
-
Perplexing Presentations (PP) and Fabricated or Induced Illness (FII) in Children
https://westyorkscb.proceduresonline.com/p_fab_ind_ill.html
Health Conditions in Schools Alliance
-
Working collaboratively to keep children with medical conditions safe in school
http://medicalconditionsatschool.org.uk/